High cholesterol symptoms and causes and levels
Find out the facts about high cholesterol, including symptoms, causes, and treatments to lower your cholesterol level.
High cholesterol refers to having an excess of cholesterol in your bloodstream, which increases your risk of heart attack or stroke.
This page answers the most frequently asked questions about high cholesterol, including the following:
- Why cholesterol is high?
- Reasons for elevated cholesterol levels?
- Types of cholesterol and markers of elevated cholesterol levels?
- Taking a cholesterol test?
- Preventive measures, both primary and secondary?
- Levels of cholesterol?
- Managing elevated cholesterol?
- Heart Helpline and further resources for assistance?
Why cholesterol is high?
One of the naturally occurring fatty substances that can be seen in your blood is cholesterol. It is created in the liver and found in a few different meals. It takes cholesterol to preserve the health of our body’s cells.
High cholesterol is an excess of cholesterol in the bloodstream, which can result from various factors. Failing to take measures to lower elevated cholesterol levels may significantly elevate the risk of experiencing a heart attack or stroke.
Reasons for elevated cholesterol levels?
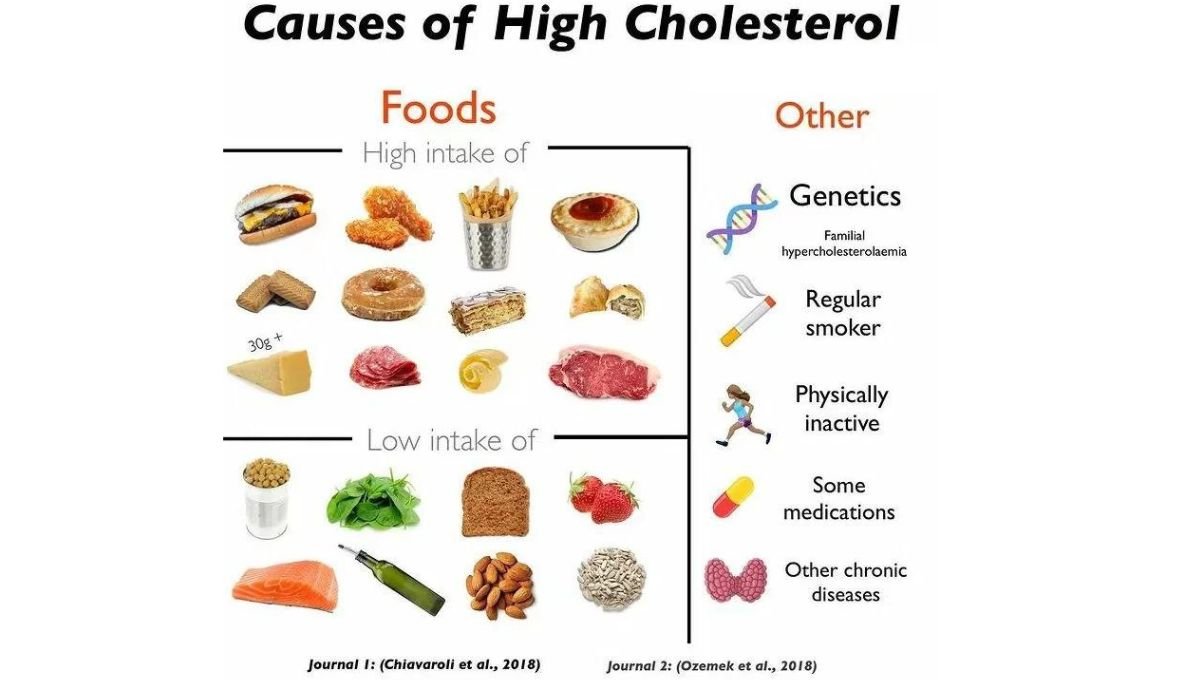 High cholesterol can occur in anyone at any time, and various circumstances can cause it. Some variables are within your control, while others are beyond your control.
High cholesterol can occur in anyone at any time, and various circumstances can cause it. Some variables are within your control, while others are beyond your control.
Some of the causes of high cholesterol that are within your control include the following:
Your lifestyle
- Consuming too much-saturated fat hampers the liver’s ability to remove cholesterol efficiently, resulting in higher cholesterol levels in the bloodstream.
- Being physically inactive – being physically active allows for an increase in the level of “good” cholesterol while simultaneously lowering the level of “bad” cholesterol.
- When you smoke, you increase the amount of tar that builds up in your arteries, which makes it easier for cholesterol to adhere to the walls of your arteries.
Factors that are beyond your control that lead to elevated cholesterol:
Your ethnic heritage, age, and biological sex
- The process of ageing – the likelihood of having higher cholesterol increases as we get older
- Males are more likely to have high cholesterol levels than females—this is especially true if your biological sex is male (you were assigned male at birth).
- You are more likely to have high cholesterol if you come from a South Asian background. This is because of your ethnic background.
Your genes
Genes hold the information that determines your features or qualities passed on to you — or inherited — from your parents. Familial hypercholesterolemia (FH) is inherited from birth through faulty genes within families. It can cause significantly elevated “lipid” levels independent of other risk factors.
Fats are transported throughout the body by lipoprotein (a), also known as LP(a), produced in the liver. High LP(a) is a disorder that can cause heart problems like heart attack and stroke. This is because LP(a) is a “sticky” substance that can accumulate in your arteries. Not only is it a disorder that is typically hereditary, but there are also other causes. Find out more through Heart UK.
Your general health
- A condition known as renal disease, in which the kidneys are not functioning correctly, can also alter how your body processes “lipid”, resulting in elevated “lipid” levels.
- Liver disease – an essential job of the liver is to produce and clear “lipid” from the body, but if the liver isn’t working well, it struggles to do this, increasing your risk of high.
- If you are someone who currently carries excess weight, particularly around your middle
- If you have type 2 diabetes, you are at greater risk of having high .
- A condition known as hypothyroidism occurs when your body does not produce enough thyroid hormone, as well as an underactive thyroid.
- Growth hormone shortage (when not enough growth hormone is generated).
Types of cholesterol and markers of elevated cholesterol levels?
Cholesterol is essential for the health of all cells in the body, as it plays a crucial role in maintaining their structure and function. Proteins in your blood flow are responsible for transporting it throughout your body to the required cells. Proteins are substances in your body that do most of the work in your cells and help maintain your body’s tissues and organs working as they should.
The results of the combination of cholesterol and proteins are referred to as lipoproteins. Lipoproteins can be broken down into two primary categories. One is terrible for your health; the other is excellent.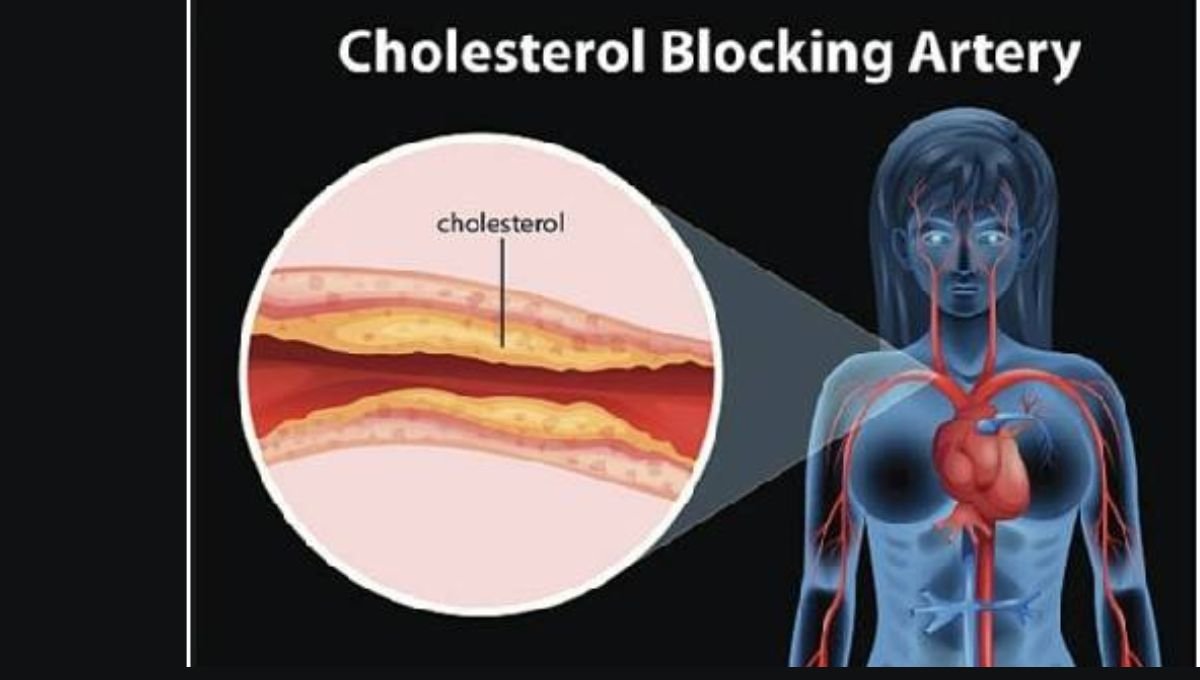
High-density lipoproteins or HDL,
It is known as ‘good’ cholesterol. It accomplishes this by transporting cholesterol that is not needed to the liver, where it is broken down and eliminated from the body. This process leads to the elimination of the “bad” cholesterol that is present in your blood.
Non-high-density lipoproteins or non-HDL are known as ‘bad’ cholesterol. Too much non-HDL leads to a build-up of fatty deposits inside the walls of the blood vessels (channels that transmit blood throughout your body). This builds up and narrows blood vessels, increasing the risk of a heart attack or stroke.
LDL (Low-Density Lipoprotein) cholesterol</strong>. In the past, LDL was viewed as the primary marker of harmful cholesterol types. However, we now recognize that other forms of non-HDL, such as VLDL (Very Low-Density Lipoprotein) and other lipid components, also significantly affect overall health. These components contribute to cardiovascular risks beyond LDL alone. Understanding these different types of “lipids”is crucial for effectively assessing and managing cardiovascular health.
Triglycerides
Elevated levels of triglycerides can contribute to the narrowing of arteries. Factors that can increase triglyceride levels include being overweight, consuming high-fat and high-sugar foods, and excessive alcohol consumption.
If your lipid profile test has shown elevated triglyceride levels, your doctor can advise you on whether they are excessively high.
You can have an average HDL and non-HDL “lipid” level yet still have a high triglyceride level. If you are found to have this, you may speak to your GP to explore what it means for you.
signs</a> of elevated cholesterol?
 High “lipid”often does not show any noticeable symptoms. Nevertheless, if it remains untreated, it substantially raises the risk of experiencing a heart attack or stroke.
High “lipid”often does not show any noticeable symptoms. Nevertheless, if it remains untreated, it substantially raises the risk of experiencing a heart attack or stroke.
Since high “lipid” is often a hidden risk factor, it can develop without our awareness until it becomes critical. This underscores the importance of regularly checking your “lipid”levels.
On the other hand, if you have a family history of hypercholesterolemia, you might exhibit apparent symptoms of abnormally high”lipid”. These include the following:
Tendon xanthomata is the term for “lipid”-related swellings on the hands, knees, or Achilles tendon at the ankle’s rear.
Xanthelasmas are small, yellowish deposits of “lipid” that often appear near the inner corners of the eyes.
The white, pale ring surrounding the coloured iris of your eye is called the corneal arcus.
<strong>Taking a cholesterol test?
 You might request that your primary care physician examine your cholesterol levels, which a straightforward blood test can determine. It is sometimes referred to as a ‘lipid profile.’ Your GP or practice nurse will take a blood sample to screen for the following:
You might request that your primary care physician examine your cholesterol levels, which a straightforward blood test can determine. It is sometimes referred to as a ‘lipid profile.’ Your GP or practice nurse will take a blood sample to screen for the following:
- levels of good “lipid”(HDL)
- levels of bad “lipid” (non-HDL)
- triglycerides
In addition, you will receive a total “lipid” result.
You might also be offered a finger-prick cholesterol test, which can be performed in certain pharmacies or as part of the National Health Service Health Check in England.
Although “lipid” levels differ from person to person, a healthy heart generally requires a low level of non-HDL and a higher level of HDL.
Preventive measures, both primary and secondary
When discussing “lipid”with your physician, you might hear the terms “primary prevention” and “secondary prevention” mentioned.
The term “primary prevention” refers to changing one’s lifestyle to prevent the development of a heart condition or the occurrence of a heart attack or stroke. These changes typically encompass lifestyle modifications such as increasing the amount of physical activity one engages in and improving one’s diet. Sometimes, doctors prescribe medications such as statins to individuals.
“Secondary prevention” is the process of modifying one’s lifestyle to prevent the progression of a heart condition or the occurrence of a subsequent event, such as a heart attack, when one already has a heart condition. This may include lifestyle changes like eating better, exercising, and taking medications such as statins.
Your doctor may suggest additional medications to further reduce your “lipid” levels. Your doctor might recommend this if your lipid levels remain high despite taking statins for a while. It could also be considered even if your current lipid levels are currently well-managed.
<strong>Levels of cholesterol</strong>
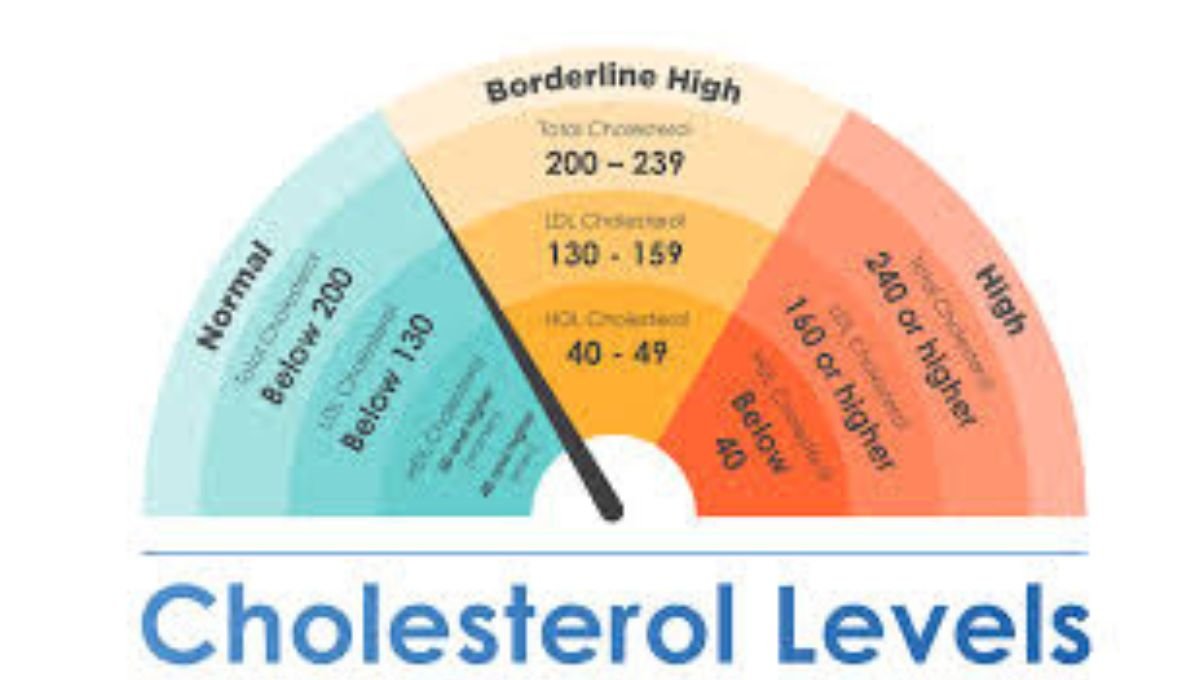
This guideline serves as an initial indicator. Your risk level depends on the specifics of your results. It’s crucial to discuss your”lipid” levels and desired targets with your physician for personalized guidance. Learn more about the significance of your results, how your doctor determines your risk, and whether you may require treatment.
<td>5 or below</table>If you have high cholesterol, it indicates an excess of “bad” cholesterol in your bloodstream, increasing the risk of heart attack or stroke. Guidelines for secondary prevention treatment of heart conditions recommend targeting specific levels for LDL-cholesterol and non-HDL lipids: LDL cholesterol should be 2.0 mmol/L or less, and non-HDL lipids should be 2.6 mmol/L or less. If you are still determining the levels you should aim for, consult your doctor.<strong>Managing elevated cholesterol</strong>There are numerous things you may do to reduce your :
- Increase your physical activity since this can not only assist in lowering your “lipid”, improve your sleep quality, and give you more energy.
- You can give up smoking and drink less alcohol.
- You might enjoy experimenting with heart-healthy dishes and meals.
- How can I get my “lipid” down? Your top five queries addressed
Your doctor can recommend medication to treat your high “lipid” if lifestyle modifications are insufficient. If you have been diagnosed with high lipid levels, your general practitioner should schedule a yearly blood test to monitor your levels and make necessary adjustments to your treatment plan.Statins constitute the most common class of medications prescribed to reduce lipid levels. However, alternative therapies are accessible. Your doctor will let you know if you need additional medications to help regulate your lipid levels. In addition, they recommend that you speak with a lipidologist. Speak with your physician or call our Heart Helpline if you have any queries concerning your medications. For additional details, could you take a look at our publications?
Heart Helpline and further resources for assistance
You qualify for an NHS health check if you are between 40 and 74 and reside in England. Your doctor must inform you about this opportunity every five years. It’s important to understand that having high lipid levels is a common issue.. Seek assistance from healthcare professionals and your family.
- Visit the Heart Helpline between 9 a.m. and 5 p.m., Monday through Friday, to speak with our cardiac nurses via phone, callback, email, or online chat.
- Please contact us if you would like to speak with our customer service representatives, locate your nearest BHF shop, and provide any feedback, compliments, or complaints we may have.
- When you sign up for our Heart Matters magazine, you will get access to online content packed with tips on health and lifestyle.
| Result | Healthy level (mmol/L) |
| Total cholesterol</td> | |
| HDL (good cholesterol) | 1 or above</td> |
| Non-HDL (bad cholesterol) | 4 or below |
| Fasting triglycerides (when you’re asked not to eat for several hours before the test) | 1.7 or below |
| Non-fasting triglycerides (when you eat as normal before the test) | 2.3 or below |
| The ideal target for the total”lipid” to HDL cholesterol ratio | 6 or below |
